Table 2: Side effects of treatment and estimated probabilities of occurrence
Side Effects of Intravesical Agents
Frequent urination
Painful urination
Flu-like symptoms
Fever or chills
Systemic infections
Skin rash
Suppression of bone marrow activity
Recent studies have indicated a possible benefit of reducing recurrences by instilling these chemicals into the bladder immediately following resection of a bladder tumor, typically in the recovery room. BCG is not used in this way because of the risk that it might be absorbed into the bloodstream in this setting.
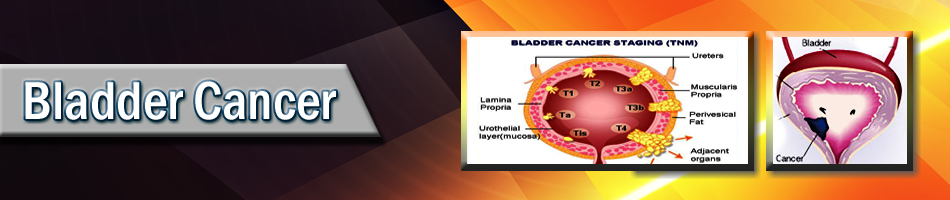
Once the grade and stage of the tumor has been determined, the urologist may decide to initiate a course of intravesical therapy with these agents. Generally, BCG is chosen if either stage T1 or carcinoma in situ is present. These patients are at highest risk of recurrence and progression and BCG is the most effective agent for preventing these adverse events. In general, Mitomycin is used for stage Ta tumors. Indications for these treatments are based upon the number of tumors that were present, their size, their appearance, the grade of tumor, and whether or not they penetrated the wall of the bladder (but not including the muscle layer). In general, six weekly treatments are given, in which a catheter is placed in the bladder, the medication is instilled, the catheter is removed, and the patient is instructed not to urinate for at least an hour.
Once the bladder has been assessed as free of disease at the first three month post-treatment cystoscopic inspection, many physicians consider it appropriate to apply additional treatments of these same drugs to forestall or prevent future recurrences. While recent studies demonstrate this concept of "maintenance therapy" is useful for some patients receiving BCG, it is of less certain benefit for those receiving the other three chemotherapeutic drugs. Whether additional treatments are given or not, periodic cystoscopies are required to detect tumor recurrence early, if it is going to develop. During the first one to two years surveillance is carried out on a quarterly basis but then can gradually be reduced to twice and eventually even once per year thereafter.
Cystectomy: Surgical removal of the bladder may be an option for patients with CIS or high-grade T1 cancers that have persisted or recurred after initial intravesical treatment. There is a substantial risk of progression to muscle-invasive cancer in such cases, and some patients may want to consider cystectomy as a first choice of treatment. If so, they should ask their doctor for information about both the risks of cystectomy and the methods of urinary reconstruction ("urinary diversion").
An alternative is to repeat intravesical therapy. There is some evidence that patients may respond to repeat therapy. However, the evidence is too weak to draw firm conclusions about whether any amount or type of intravesical therapy, in any combination, can affect progression of high-grade disease. Patients with high risk disease, such as high grade TA or T1 cancer or CIS, who fail BCG are at particularly high risk and should strongly consider radical cystectomy.
Frequently asked questions:
Do bladder tumors occur in children?
Fortunately, bladder tumors are rare in children.
What are some risk factors for bladder cancer?
Smokers develop bladder cancer at two to three times the rate of non-smokers. People who work with dyes, metal, paints, leather, textile and organic chemicals may be at a higher risk. People who have chronic bladder infections may also be at higher risk.
Is there a screening test for early detection of bladder cancer?
Not at this time, although periodic check of the urine for microscopic blood may promote earlier detection. |